The right tool for the right patient: Resuscitative TEE in the diagnosis of massive PE in the ED
by tom jelic
We have multiple tools in the ED that allow us to assess patients rapidly. But of course, you must use the right tool for the patient. Transthoracic echo (TTE) can be useful to assess a patient in shock and is our go-to tool when we approach a patient with hemodynamic decompensation or shock. But what happens when TTE fails you? What happens if TTE views are not obtainable or suboptimally to make any informed clinical decisions off of? How do you ensure you meet the standard of care and obtain the information you need to make decisions?. In this post we share a case highlighting how TEE can play a pivotal role in resuscitative medicine, especially when TTE fails in the evaluation of a patient with rapid hemodynamic decompensation.
An 86 year old female with a history of hypertension was brought to the ED with shortness of breath. EMS found her to be in atrial fibrillation with rapid ventricular response. Shortly after arrival, the patient decompensated and arrested. She was intubated quickly, and standard ACLS care was provided for a PEA arrest. An arterial line was placed, and a TTE was performed. The only issue was the TTE could not yield adequate images from any cardiac imaging vantage point. The patient had ROSC, but remained hemodynamically unstable. A TEE was deployed during this arrest using a focused TEE assessment and yielded superior views. In Clip 1, a mid-esophageal 4 chamber view was obtained by simply inserting the probe and advancing it until the view is obtained. In this view, we noted the left ventricle (LV) appeared underfilled and hyperdynamic. The right ventricle appeared slightly enlarged, but we need more views.
In Clip 2, a mid-esopahageal right ventricular inflow-outflow view is obtained. This view demonstrated an enlarged RV. In Clip 3, color doppler is placed over the tricuspid valve, exhibiting moderate to severe tricuspid regurgitation. In Clip 4, a mid-esophageal long axis view shows a hyperdynamic LV and no evidence proximal aortic root pathology. Clip 5 shows a transgastric short axis view, demonstrating an enlarged RV, interventricular septal bowing and an empty, hyperdynamic LV.
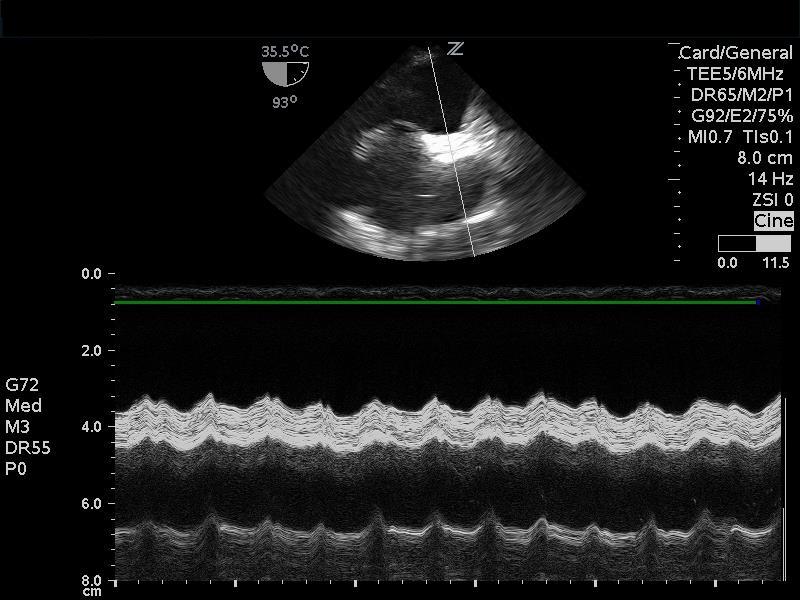
Things seemed to be coming together; an empty, hyperdynamic LV, an enlarged RV with moderate to severe tricuspid regurgitation, all consistent with elevated RV pressures. We rapidly moved on to an assessment of the SVC in image 6.
image 6. m-mode through svc in bicaval view
The M-mode tracing above demonstrates an SVC that is plethoric with no respirophasic changes. The TEE findings all pointed to a very high suspicion of pulmonary embolism causing the patients clinical presentation.
After initiating vasopressors, the patient stabilized enough to undergo a CT chest, which confirmed massive PE.
The frequency of inadequate image acquisition from an emergency medicine perspective is unknown. However, from a study by Vignon et al. in a critical care population, TTE was only able to provide adequate images in 38% of cases (1). The same study showed that TEE aided in 98% of clinical decisions and had a significantly higher impact on patient care than TTE. An observational study of focused TEE performed in the ED by Arntfield et al. revealed a 98% success rate in image acquisition (2). It also showed that no complications occurred from the placement of the TEE probe. The focused TEE assessment in this single observational study also showed the TEE use was diagnostically and clinically useful in 78% of cases.
This case highlights that TEE can play a vital role and add another tool in the resuscitationist's arsenal.
References
1. Vignon P, Mentec H, Terre S, et al. Diagnostic accuracy and thera- peutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest 1994;106: 1829–34
2. Arntfield R, Pace J, Hewak M, et al. Focused transesophageal echo- cardiography by emergency physicians is feasible and clinically influential: observational results from a novel ultrasound program. J Emerg Med 2016;50:286–94.
*this case was published in journal of emergency medicine in november 2017*
citation: Jelic T, Baimel M, Chenkin J. Bedside Identification of Massive Pulmonary
Embolism with Point-of-Care Transesophageal Echocardiography. J Emerg Med. 2017
Nov;53(5):722-725. PubMed PMID: 29128035